Search
- Page Path
- HOME > Search
- Thyroid
- Evaluation of Iodine Status among Korean Patients with Papillary Thyroid Cancer Using Dietary and Urinary Iodine
- Ji Yeon Choi, Joon-Hyop Lee, YoonJu Song
- Endocrinol Metab. 2021;36(3):607-618. Published online June 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1005
- 3,924 View
- 122 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Concerns have been raised regarding thyroid disorders caused by excessive iodine in Koreans, who have iodine-rich diets. This study evaluated iodine status using dietary iodine intake and urinary iodine in papillary thyroid cancer (PTC) patients.
Methods
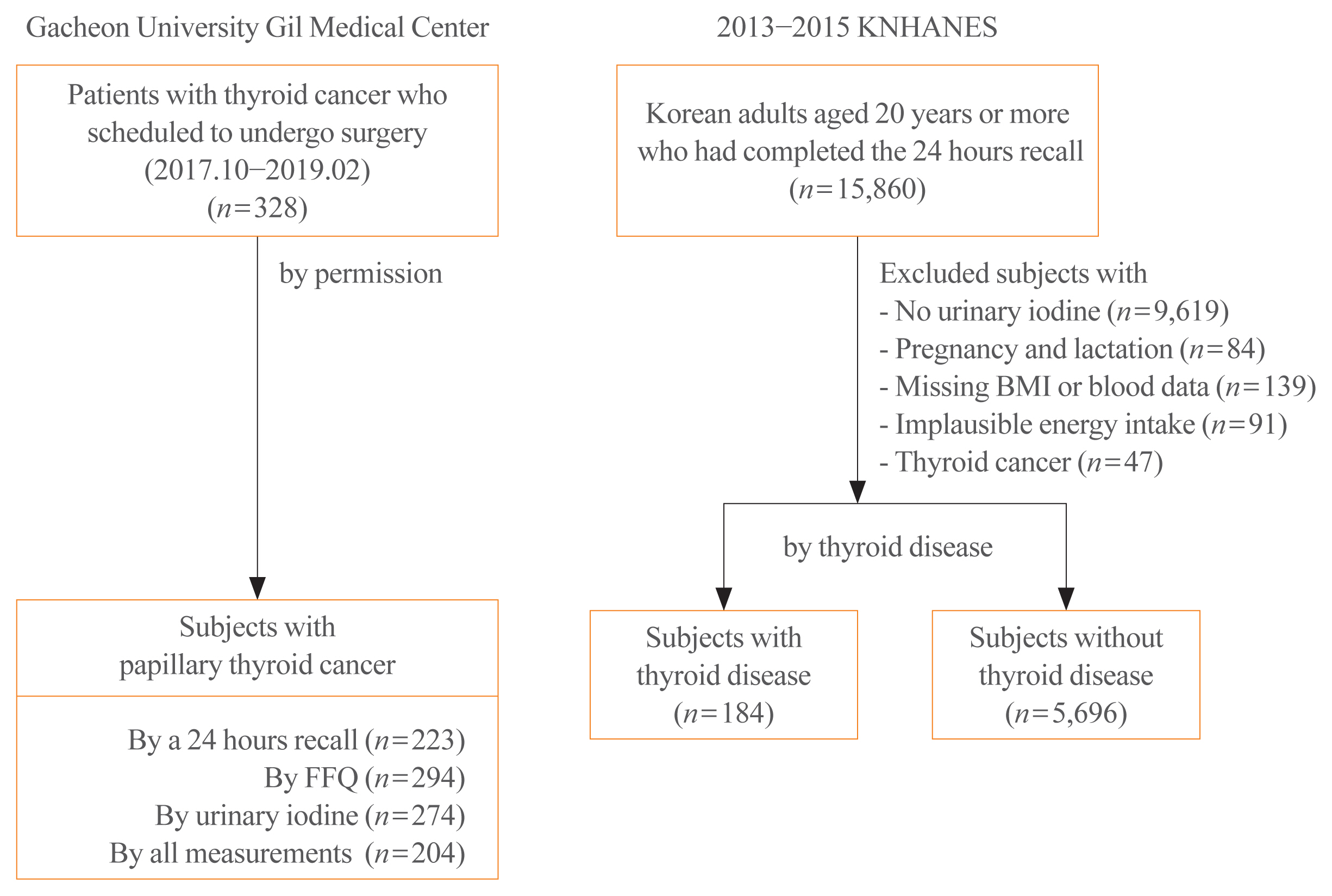
Dietary data of PTC patients were assessed using a 24-hour recall and food frequency questionnaire (FFQ), and urinary iodine concentrations (UICs) were also obtained. To compare the iodine status of PTC patients, Korean adults with or without thyroid disease from the Korea National Health and Nutrition Examination Survey, which had 24-hour recall data and urinary iodine measurements, were analyzed.
Results
The median daily iodine intake by 24-hour recall was 341.7 μg/day in PTC patients, similar to the levels of other Korean adults. Based on UICs, the prevalence of excessive iodine was 54.4% in PTC patients, which was similar to the prevalence among subjects with thyroid disease (55.4%) but slightly higher than that in subjects without thyroid disease (47.7%). Based on dietary iodine by 24-hour recall, the prevalence of excessive iodine intake was 7.2%, which was higher than that among subjects with (4.4%) or without (3.9%) thyroid disease. The dietary iodine intake based on 24-hour recall was closely correlated with the UIC (r=0.4826) in PTC patients, but dietary iodine by FFQ was not significantly correlated with either 24-hour recall or UIC-based dietary iodine.
Conclusion
Excessive iodine intake was more common in PTC patients than in subjects without thyroid disease. Further longitudinal research is necessary to elucidate the role of dietary iodine in PTC. -
Citations
Citations to this article as recorded by- Association between iodine nutrition and cervical lymph node metastasis of papillary thyroid microcarcinoma
Hengqiang Zhao, Jin Hu, Le Cui, Yiping Gong, Tao Huang
Frontiers in Endocrinology.2023;[Epub] CrossRef - Effect of iodine restriction on short-term changes in thyroid function in patients with subclinical hypothyroidism
Obin Kwon, Dong Yeob Shin, Eun Jig Lee
Journal of Nutrition and Health.2022; 55(2): 250. CrossRef - Iodine nutrition and papillary thyroid cancer
Xueqi Zhang, Fan Zhang, Qiuxian Li, Chuyao Feng, Weiping Teng
Frontiers in Nutrition.2022;[Epub] CrossRef
- Association between iodine nutrition and cervical lymph node metastasis of papillary thyroid microcarcinoma

- Thyroid
- Effect of Cigarette Smoking on Thyroid Cancer: Meta-Analysis
- Joon-Hyop Lee, Young Jun Chai, Ka Hee Yi
- Endocrinol Metab. 2021;36(3):590-598. Published online May 26, 2021
- DOI: https://doi.org/10.3803/EnM.2021.954
- 12,970 View
- 191 Download
- 8 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Although smoking is generally carcinogenic, its effect on thyroid cancers is still subject to controversy. The purpose of this study was to summarize the role of smoking in relation to thyroid cancer occurrence.
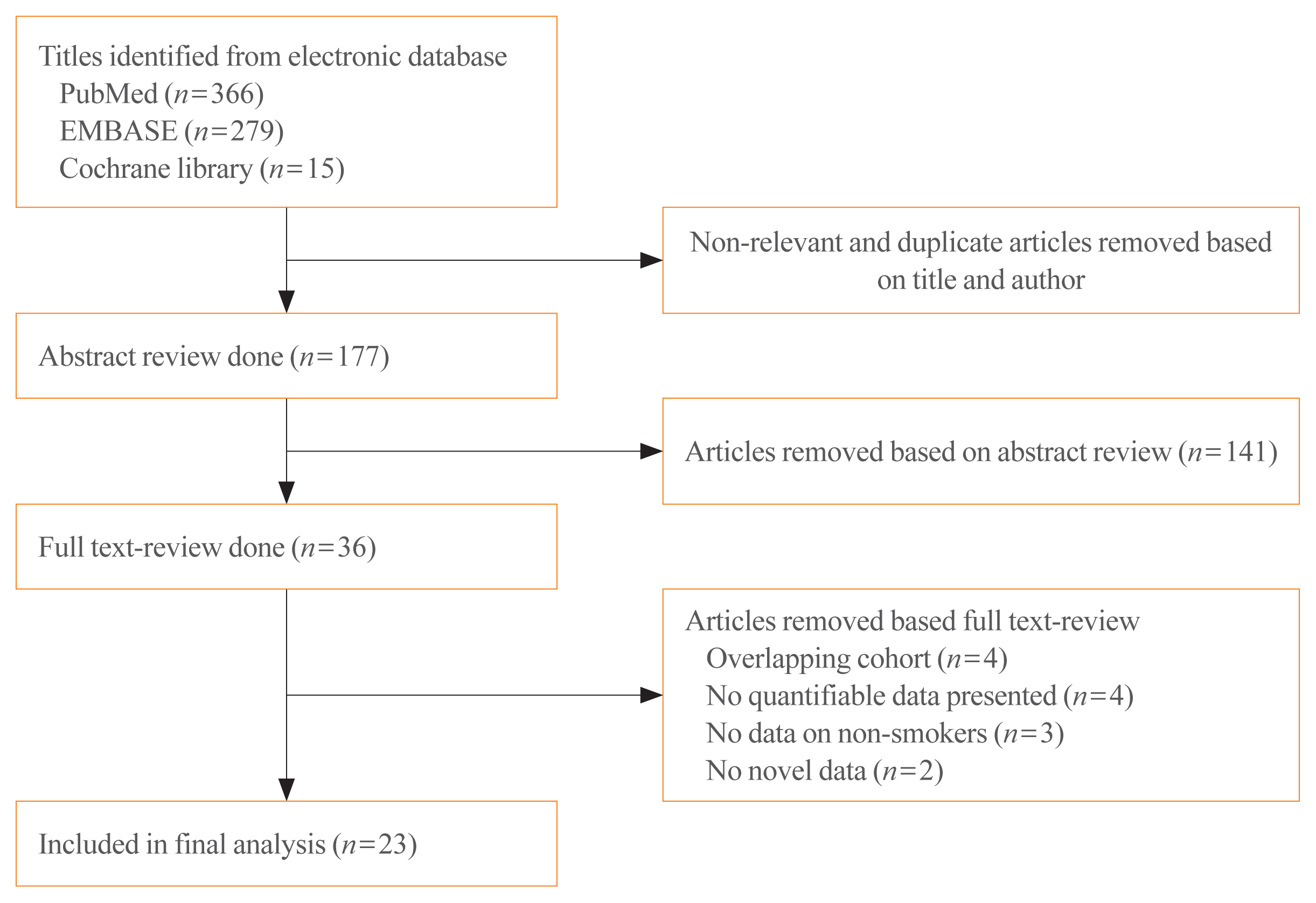
Methods
We performed a meta-analysis of 24 eligible studies: 21 case-control studies and three prospective cohort studies. The summary odds ratio (OR) and 95% confidence interval (CI) of all studies were acquired based on random effect model. Further subgroup analyses were conducted according to gender, histological type of thyroid cancer, and smoking status of patients for the case-control studies.
Results
The summary effect size indicated a negative association of smoking for thyroid cancer (OR, 0.798; 95% CI, 0.681 to 0.935). From the subgroup analyses for the case-control studies, reduced risk of thyroid cancer was observed in both men (OR, 0.734; 95% CI, 0.553 to 0.974) and women (OR, 0.792; 95% CI, 0.700 to 0.897). The protective effect of smoking was observed in studies in which thyroid cancer was limited to differentiated thyroid cancers (DTCs) (OR, 0.798; 95% CI, 0.706 to 0.902).
Conclusion
Our results suggests that smoking may have a protective effect on thyroid cancer, especially on DTCs. Further studies with larger sample sizes should be conducted in elucidating the dose and time dependent effect of smoking on thyroid cancer with specific focus on the types of thyroid cancers. -
Citations
Citations to this article as recorded by- Tobacco smoking, e-cigarette and thyroid: what are the risks of thyroid disorders
I. M. Belovalova, E. S. Shugurova, M. O. Korchagina, T. N. Borkhoeva, M. S. Sheremeta
Clinical and experimental thyroidology.2024; 19(2): 11. CrossRef - Relationship between Serum Levels of Selenium and Thyroid Cancer: A Systematic Review and Meta-Analysis
Runhua Hao, Ping Yu, Lanlan Gui, Niannian Wang, Da Pan, Shaokang Wang
Nutrition and Cancer.2023; 75(1): 14. CrossRef - Potentially inappropriate medication and frailty in older adults: A systematic review and meta-analysis
Wenlian Ma, Hongyan Wang, Zhifei Wen, Linfeng Liu, Xiangeng Zhang
Archives of Gerontology and Geriatrics.2023; 114: 105087. CrossRef - Inflammation biomarkers are associated with the incidence of cardiovascular disease: a meta-analysis
Yifei Liu, Suzhen Guan, Haiming Xu, Na Zhang, Min Huang, Zhihong Liu
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Maternal gestational weight gain and offspring’s neurodevelopmental outcomes: A systematic review and meta-analysis
Dan Wu, Yicheng Li, Lingyan Chen, Marieke Klein, Barbara Franke, Jinjin Chen, Jan Buitelaar
Neuroscience & Biobehavioral Reviews.2023; 153: 105360. CrossRef - Association of preoperative hypoprotein malnutrition with spinal postoperative complications and other conditions: A systematic review and meta-analysis
Yongrong Hu, Liping Wang, Hao Liu, Kunhai Yang, Song Wang, Xiang Zhang, Bo Qu, Hongsheng Yang
Clinical Nutrition ESPEN.2023; 57: 448. CrossRef - Metabolic syndrome and risk of ovarian cancer: a systematic review and meta-analysis
Ziyu Chen, Zesi Liu, Hongxia Yang, Chaosheng Liu, Fandou Kong
Frontiers in Endocrinology.2023;[Epub] CrossRef - Cigarette smoking and thyroid cancer risk: A Mendelian randomization study
Hongzhan Jiang, Yi Li, Jiali Shen, Huihui Lin, Siyue Fan, Rongliang Qiu, Jiaxi He, Ende Lin, Lijuan Chen
Cancer Medicine.2023; 12(19): 19866. CrossRef - Longitudinal Changes in Smoking Habits in Women and Subsequent Risk of Cancer
Thi Xuan Mai Tran, Soyeoun Kim, Huiyeon Song, Boyoung Park
American Journal of Preventive Medicine.2022; 63(6): 894. CrossRef
- Tobacco smoking, e-cigarette and thyroid: what are the risks of thyroid disorders

- Miscellaneous
- Rare PTH Gene Mutations Causing Parathyroid Disorders: A Review
- Joon-Hyop Lee, Munkhtugs Davaatseren, Sihoon Lee
- Endocrinol Metab. 2020;35(1):64-70. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.64

- 5,105 View
- 108 Download
- 8 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Since parathyroid hormone (PTH) was first isolated and its gene (
PTH ) was sequenced, only eightPTH mutations have been discovered. The C18R mutation inPTH , discovered in 1990, was the first to be reported. This autosomal dominant mutation induces endoplasmic reticulum stress and subsequent apoptosis in parathyroid cells. The next mutation, which was reported in 1992, is associated with exon skipping. The substitution of G with C in the first nucleotide of the second intron results in the exclusion of the second exon; since this exon includes the initiation codon, translation initiation is prevented. An S23P mutation and an S23X mutation at the same residue were reported in 1999 and 2012, respectively. Both mutations resulted in hypoparathyroidism. In 2008, a somatic R83X mutation was detected in a parathyroid adenoma tissue sample collected from a patient with hyperparathyroidism. In 2013, a heterozygous p.Met1_Asp6del mutation was incidentally discovered in a case-control study. Two years later, the R56C mutation was reported; this is the only reported hypoparathyroidism-causing mutation in the mature bioactive part ofPTH . In 2017, another heterozygous mutation, M14K, was detected. The discovery of these eight mutations in thePTH gene has provided insights into its function and broadened our understanding of the molecular mechanisms underlying mutation progression. Further attempts to detect other such mutations will help elucidate the functions of PTH in a more sophisticated manner.-
Citations
Citations to this article as recorded by- The Intricacies of Renal Phosphate Reabsorption—An Overview
Valerie Walker
International Journal of Molecular Sciences.2024; 25(9): 4684. CrossRef - Molecular and Clinical Spectrum of Primary Hyperparathyroidism
Smita Jha, William F Simonds
Endocrine Reviews.2023; 44(5): 779. CrossRef - Rare cause of persistent hypocalcaemia in infancy due to PTH gene mutation
Savita Khadse, Vrushali Satish Takalikar, Radha Ghildiyal, Nikhil Shah
BMJ Case Reports.2023; 16(9): e256358. CrossRef - Homozygous Ser-1 to Pro-1 mutation in parathyroid hormone identified in hypocalcemic patients results in secretion of a biologically inactive pro-hormone
Patrick Hanna, Ashok Khatri, Shawn Choi, Severine Brabant, Matti L. Gild, Marie L. Piketty, Bruno Francou, Dominique Prié, John T. Potts, Roderick J. Clifton-Bligh, Agnès Linglart, Thomas J. Gardella, Harald Jüppner
Proceedings of the National Academy of Sciences.2023;[Epub] CrossRef - Genetics of monogenic disorders of calcium and bone metabolism
Paul J. Newey, Fadil M. Hannan, Abbie Wilson, Rajesh V. Thakker
Clinical Endocrinology.2022; 97(4): 483. CrossRef - Homozygous missense variant of PTH (c.166C>T, p.(Arg56Cys)) as the cause of familial isolated hypoparathyroidism in a three-year-old child
Stine Linding Andersen, Anja Lisbeth Frederiksen, Astrid Bruun Rasmussen, Mette Madsen, Ann-Margrethe Rønholt Christensen
Journal of Pediatric Endocrinology and Metabolism.2022; 35(5): 691. CrossRef - Novel PTH Gene Mutations Causing Isolated Hypoparathyroidism
Colin P Hawkes, Jamal M Al Jubeh, Dong Li, Susan E Tucker, Tara Rajiyah, Michael A Levine
The Journal of Clinical Endocrinology & Metabolism.2022; 107(6): e2449. CrossRef
- The Intricacies of Renal Phosphate Reabsorption—An Overview


 KES
KES

 First
First Prev
Prev



